Skip to main content
Notes
table of contents
Chapter 5
eHealth Economic Evaluation Framework
Francis Lau
5.1 Introduction
Increasingly, healthcare organizations are challenged to demonstrate the worth
of eHealth investments with respect to their economic return. Over the years,
different approaches have been applied to determine the value of eHealth
investments such as the financial benefit, cost-effectiveness and
quality-adjusted life years gained. Despite the work done to date, there is
still limited evidence on the economic return associated with the myriad of
eHealth systems deployed. This available evidence is often mixed as to whether
eHealth can demonstrate a positive return on the investment or not. Moreover,
the methodological rigour of some evaluation studies is questionable.
In 2013, Bassi and Lau published a scoping review of primary studies on the
economic evaluation of HIS or health information systems (2013). Based on 33 high-quality HIS economic evaluation studies published between 2000 and 2012 we reported on the
key components of an HIS economic evaluation study, the current state of evidence on economic return of HIS, and a set of guidance criteria for conducting HIS economic evaluation studies. Drawing on the review findings, we proposed an
economic evaluation classification scheme that is the basis of the eHealth
Economic Evaluation Framework described in this chapter.
This chapter describes an eHealth Economic Evaluation Framework based on our
scoping review findings and related best practices in economic evaluation
literature. The chapter covers the underlying conceptual foundations and the
six dimensions of our framework, guidance on its potential use and implications
for healthcare organizations.
5.2 Conceptual Foundations
Different economic evaluation approaches for eHealth have been described in the
literature. They vary according to the analytical methods applied, the health
consequences being considered, and whether it involves a synthesis of multiple
studies. The quality of eHealth economic evaluation studies also varies
depending on the methodological rigour applied in their design, analysis and
reporting. The type and quality of eHealth economic evaluation studies are
described below.
5.2.1 Types of Economic Evaluation in eHealth
Economic evaluation is the comparative analysis of alternative interventions
with respect to their costs and consequences. Economic evaluation can be based
on empirical trials, mathematical models, or a combination of both. The types
of economic evaluation studies found in eHealth literature include cost-benefit
analysis, cost-effectiveness analysis, and cost-utility analysis. Other
variants are cost-minimization analysis, cost-consequence analysis, input cost
analysis, and cost-related outcome analysis. These types of economic evaluation
are defined below (Roberts, 2006).
- Cost-benefit analysis – examines both costs and consequences in monetary terms.
- Cost-effectiveness analysis – examines costs and a single consequence in its natural unit such as hospital length of stay in days or frequency of adverse events as a percentage.
- Cost-utility analysis – examines costs and a single consequence in the form of a health-related quality of life measure such as quality-adjusted life years.
- Cost-consequence analysis – examines the costs and multiple consequences in their natural units without aggregation into a single consequence.
- Cost-minimization analysis – examines the least costly consequence among alternatives with equivalent consequences.
- Input cost analysis – examines the costs of all alternatives but not their consequences.
- Cost-related outcome analysis – examines the consequences of all alternatives in monetary terms but not the input costs incurred.
When the economic analysis involves the comparison of both the costs and
consequences, it is considered a full economic evaluation. Cost-benefit,
cost-effectiveness, cost-utility, and cost-consequence analyses are examples of
full economic evaluation. If the analysis involves only the costs (e.g., input
cost analysis) or consequences (e.g., cost-related outcome analysis), it is
considered a partial or one-sided economic evaluation. Cost-minimization is a
form of input cost analysis since it assumes all of the consequences are
equivalent and therefore the focus is on the least costly alternative.
In the eHealth literature, sometimes the term “benefit” is used to include different types of consequences which may be non-monetary in
nature. An example is the term “benefits evaluation” where the benefits can be in dollar terms or in some other units such as
hospital length of stay in days or number of adverse events in a given time
period. To avoid confusion it is important to describe the type of economic
analysis used and the nature of the benefits involved.
5.2.2 Quality of eHealth Economic Evaluation Studies
Different criteria for assessing the quality of economic evaluation studies in
terms of their design, analysis and reporting have been published in the
literature. In this section, we briefly describe the quality assessment
criteria from our scoping review and the Consolidated Health Economic
Evaluation Reporting Standards (CHEERS) publication guidelines (Husereau et al., 2013) as two ways to enhance the
rigour of our eHealth Economic Evaluation Framework. These are described in
more detail in chapter 14 under methodological considerations and best practice
guidelines.
Ten quality criteria derived from four literature sources were used in our
scoping review to assess the methodological quality of the selected HIS economic evaluation studies (Drummond & Jefferson, 1996; Centre for Reviews and Dissemination [CRD], 2009; Evers, Goossens, de Vet, van Tulder, & Ament, 2005; Machado, Iskedjian, & Einarson, 2006). Each criterion scores between 0 and 1, from not stated,
somewhat stated, to clearly stated, for a maximum score of 10 as having the
highest quality. These criteria are listed below:
- Is there a research question or definition of the study aim?
- Are the primary outcome measures stated?
- Is the study sample provided and described?
- Is the HIS being evaluated described?
- Is the study time horizon stated?
- Are the data collection methods described?
- Are the analytical methods described?
- Are the results clearly reported with caveats where needed?
- Do the conclusions follow from the study question/objective?
- Are generalizability issues addressed along with limitations?
The CHEERS guidelines were published in 2013 (Husereau et al., 2013) by the Good Reporting
Practices Task Force of the International Society for Pharmacoeconomics and
Outcomes Research (ISPOR). The guidelines are recommendations for optimized reporting of health economic
evaluation studies. They were derived from previous systemic reviews and
surveys of task force members, followed by two rounds of Delphi process that
reduced an initial list of 44 candidate reporting items to 24 items with
accompanying recommendations in a checklist format.
- Title and abstract – two items on having a title that identifies the study as an economic evaluation, and a structured summary of objectives, perspective, setting, methods, results and conclusions.
- Introduction – one item on study context and objectives, including its policy and practice relevance.
- Methods – 14 items on target populations, setting, perspective, comparators, time horizon, discount rate, choice of health outcomes, measurement of effectiveness, measurement and valuation of preference-based outcomes, approaches for estimating resources and costs, currency and conversion, model choice, assumptions, and analytic methods.
- Results – four items on study parameters, incremental costs and outcomes, describing uncertainty, and describing heterogeneity.
- Discussion – one item on findings, limitations, generalizability and current knowledge.
- Others – two items on the source of study funding and conflicts of interest.
5.3 Framework Dimensions
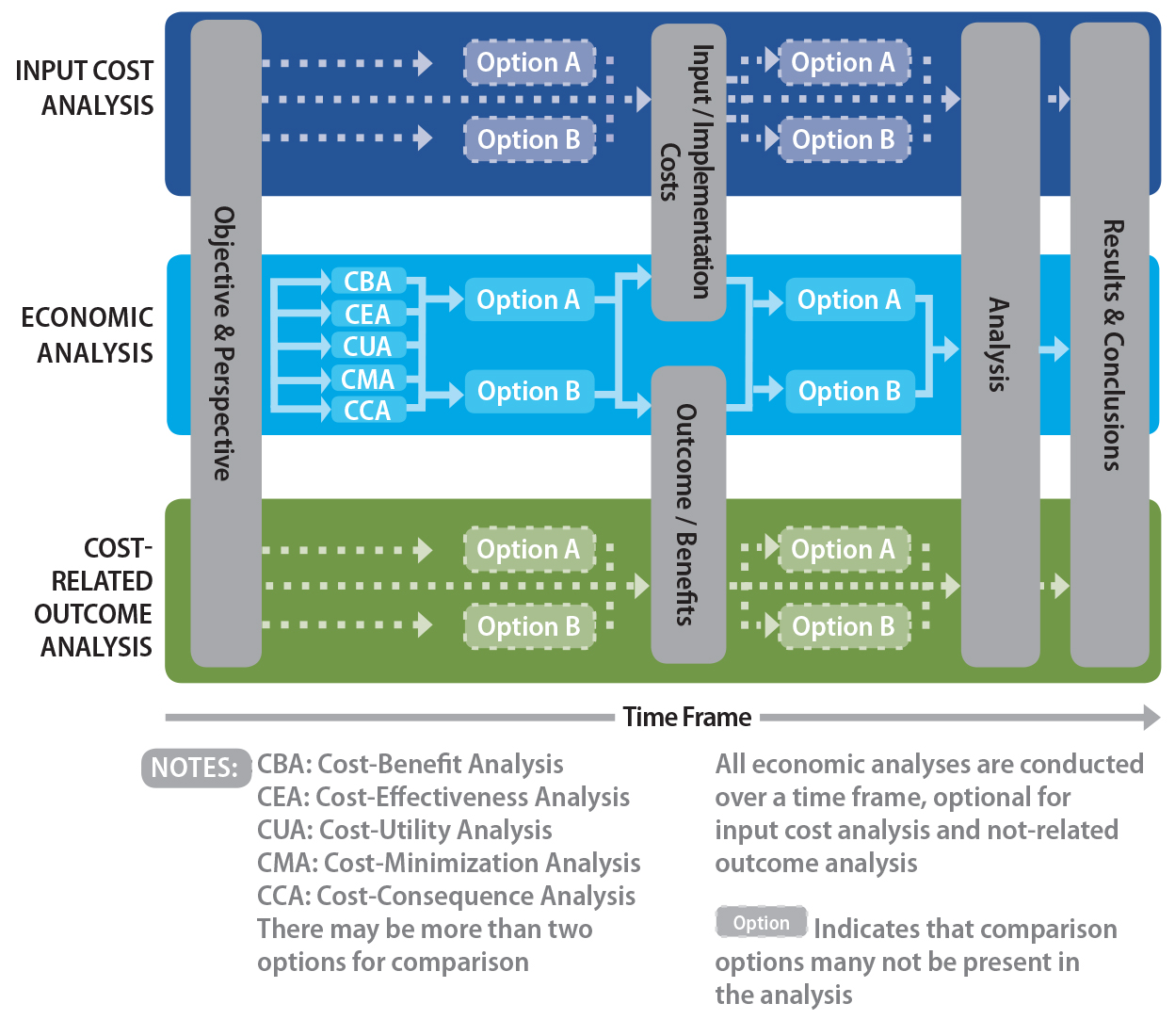
The eHealth Economic Evaluation Framework is derived from our scoping review of HIS economic evaluation studies. Its intent is to provide a classification scheme
for the different approaches used in eHealth economic evaluation studies. The
framework is made up of six components: having a perspective, options, time
frame, costs, outcomes, and method of analyzing/comparing options. These
components are shown in Figure 5.1 and described below.
Figure 5.1. eHealth economic evaluation framework.
Note.From “Measuring value for money: A scoping review on economic evaluation of health
information systems,” by J. Bassi and F. Lau, 2013, Journal of American Medical Informatics Association, 20(4), p. 793. Copyright 2013 by Oxford University Press, on behalf of American
Medical Informatics Association. Reprinted with permission.
5.3.1 Perspective
Perspective refers to the point of view under which an eHealth economic
evaluation is being conducted. It is an important component in the framework
because the costs and consequences accrued can affect different parts of the
healthcare system. As such, the economic return of an eHealth system is
dependent upon who makes the decision, who incurs the costs and who benefits
from the consequences. For instance, care providers mandated by the government
to adopt an electronic prescription tracking system may perceive it as an added
cost that only benefits the government by controlling their practice. The
perspectives considered in our framework are those of the individual,
organization, payer, and society at large. These are defined below:
- Individual – the person affected such as the provider, patient or caregiver. The effect may involve a change in the person’s expenditures, routines and/or health conditions.
- Organization – the group affected such as the health region, professional association, or patient advocacy where multiple individuals within the group are affected in similar ways.
- Payer – the group that finances the healthcare service such as the government or private insurers. The effect may involve a change in the group’s cost of providing the service.
- Society – the general public affected such as the residents in a geographic region or the entire population of a country. The effect may involve a change to the overall financing of the healthcare system and/or the health status of the population.
5.3.2 Options
Options are the alternative eHealth systems being considered. It is important to
clearly define each eHealth system option since they often perform multiple
functions and can be adopted for different reasons by different organizations.
Also, the behaviour of the system can evolve over time as users become more
experienced in using it to support their work. Increasingly, eHealth systems
are combined with other interventions to enhance the intended effects. For
these reasons, the features within each of these options must be clearly
defined for meaningful comparisons to be made. The types of options reported in
the eHealth economic evaluation literature are with or without the system, pre-
or post-implementation, types of systems, levels of systems, different time
points, and different sites. These options are defined below:
- With or without the system – one or more eHealth system options and a status quo with no system
- Pre- or post-implementation – before and after the adoption of an eHealth system
- Types of systems –different eHealth system options with the same or similar functions
- Levels of systems – extent of eHealth systems and/or functions adopted in the organization
- Different time points – the same eHealth system at different points in time
- Different sites – the same eHealth system adopted in different organizations or locations
Two important aspects of options are the status quo and opportunity cost. Status
quo refers to the costs and consequences of the current situation without
adopting any eHealth systems, or a default “do nothing” position. Opportunity cost refers to the foregone benefit as a result of
selecting a given eHealth system option. Status quo and opportunity cost are
important in eHealth investment decisions when there are limited resources
among competing priorities. For example, a healthcare organization addressing
patient medication safety has to decide whether its existing rate of medication
errors, or the status quo, is acceptable or needs improvement with an
electronic surveillance system as an option. Similarly, an organization wishing
to adopt an EMR system to improve its overall care delivery may consider the opportunity cost
by asking whether the EMR investment can be better spent elsewhere with comparable effect.
5.3.3 Time Frame
Time frame refers to the length of time for which the costs and consequences of
an eHealth system are accrued. One must allow for sufficient time to ensure all
of the relevant costs are captured and the consequences are realized as they
can accrue differently over time. Often there is a time lag before the
consequences, such as a reduction in the rate of adverse events, can be
realized after the adoption of an eHealth system. For pragmatic reasons,
studies based on empirical data for costs and consequences tend to use shorter
time frames, as it is difficult and costly to collect data for a long period.
Studies based on mathematical modelling tend to have longer time frames since
there is little added effort to predict long-term trends. The time frames
reported in eHealth economic evaluation literature are less than one year, one
to five years, six to 10 years, and greater than 10 years. They are defined
below:
- Less than one year – typically for small-scale studies where empirical data on costs and consequences from an eHealth system or intervention are collected over a short time period such as three to six months for comparison. Sometimes the cost and/or consequence are extrapolated to an annual period such as estimated cost savings from an EMR system per year.
- One to five years – the most common time periods used are between one and five years in duration to capture the costs, consequences, or both, that are accrued. Sometimes different time periods are used to collect the accrued costs and consequences. For instance one may extract the historical costs for EMR adoption over one year then estimate the return on investment over a five-year period.
- Six to 10 years – typically for modelling studies where the costs and consequences are projected over a six- to 10-year period. The data can be based on historical, prospective, estimated or combined sources.
- Greater than 10 years – mostly for predicting the long-term consequences of an eHealth system such as the cumulative economic impact of a diabetes management system expected over a 40-year period.
- Multiple time points – typically in studies where different types of costs and consequences are captured across multiple time periods depending on the availability of the data.
Note that the time period covered in an economic evaluation study is different
from the time it takes to conduct the study itself. For instance, the economic
return of a computerized provider order entry system (CPOE) may be determined over a 5-year period to ensure all of the costs incurred are
captured and the CPOE is sufficiently stabilized to realize an improvement in ordering medications.
Yet the study itself may only take two or three months to collect and analyze
the data if it is retrospective in nature or if predictive modelling is used to
estimate the effect over a five-year period based on historical data.
5.3.4 Input Costs
Input costs are the amounts of money spent in the adoption of an eHealth system.
The types of costs reported in the eHealth economic evaluation literature are
one-time direct costs, ongoing direct costs, and ongoing indirect costs. They
are defined below.
- One-time direct costs – expenditures incurred in order to implement the system. They include such items as hardware equipment, software licences, application development/customization, data conversion, system configuration, training, user and technical support.
- Ongoing direct costs – recurrent expenditures to operate the system after its implementation. They include such items as hardware and software maintenance, system upgrades, technical and support staffing, ongoing training, and related professional services (e.g., system audits).
- Ongoing indirect costs – recurrent expenditures related to the system that is allocated by the organization after its implementation. They include prorated expenditures such as managing IT-related privacy, security, policy and help desk, and changes in staff workload.
Intangible costs are another type of cost that is mentioned in the economic
evaluation literature. Intangible costs refer to things that are unquantifiable
or difficult to measure. Examples of intangible costs in the adoption of an
eHealth system are a change in staff morale and patient anxiety before, during
and after the implementation of an EMR as they learn to work with the new system. Intangible costs are seldom
addressed in eHealth economic evaluations. One approach is to estimate
intangible costs as a type of input or outcome such as the quality of staff
work life in terms of productivity before or after the adoption of an EMR.
5.3.5 Outcomes
Outcomes refer to the consequences from adopting an eHealth system. There are
different types of outcomes reported in the eHealth economic evaluation
literature. These outcomes may be financial or non-financial in nature, and can
be derived from empirical data, projections or both. Financial outcomes include
changes in revenues, labour and supply costs, and capital costs expressed in
monetary units. Non-financial outcomes include changes in resource utilization
and health outcomes in their natural units. These types of consequences are
outlined below. Note that only tangible outcomes are considered here.
- Revenues – money generated from billing and payment of patient care service provision supported by the eHealth system, and change in such financial arrangements as the reimbursement rates, accounts receivable days and payer mix for service claims.
- Labour and supply cost savings – change in staffing costs due to altered productivity associated with the eHealth system such as data entry, charting, communication and reporting, and change in supply costs such as the amount of stocked materials and goods consumed.
- Capital cost savings – change in capital expenditures for such items as facilities, equipment and technology due to the adoption of an eHealth system.
- Resource utilization – change in healthcare resource usage such as the volume of laboratory and radiology tests, medications and other diagnostic/interventional procedures consumed.
- Health outcomes – change in patients’ conditions and clinical events such as one’s physiologic status, or the number of medical errors and adverse events reported.
5.3.6 Comparison of Options
Comparison of options refers to the analytical methods used to determine the
return on investment for each eHealth system option being considered. Different
methods have been reported in the eHealth economic evaluation literature. They
include accounting, statistical, and operations research methods that draw on
different types of data as their input sources. These are defined below.
- Data sources – tabulation of cost and outcome data as the input data sources, based on historical records, expert estimates, model projections, or combinations.
- Accounting – measuring the financial performance of each option, which includes the outcome measures, time value of money, uncertainty and risks. Examples of outcome measures are incremental cost-effectiveness ratio, payback, net present value, operating margin and quality-adjusted life years. Examples of time value of money are discounting, inflation, depreciation and amortization. Examples of handling uncertainty and risks are sensitivity and scenarios analysis.
- Statistics – measuring the financial performance of each option based on statistical techniques such as linear/logistic regression, general linear modelling and testing for group differences.
- Operations research – measuring the financial performance of each option based on operational research methods such as panel regression, parametric cost analysis, stochastic frontier analysis and simulation modelling.
5.4 Framework Usage
The eHealth Economic Evaluation Framework was derived from a scoping review of
33 high-quality HIS economic evaluation studies published between 2000 and 2012. The review provides
a rich source of published studies, methods, measures, and lessons that can
serve as guidance for designing, analyzing and reporting eHealth economic
evaluation studies. The potential usage and implications of this framework
based on the six components reported in the review are described below.
5.4.1 Potential Usage
For the 33 HIS studies in the review, 12 were considered full economic evaluations as they
included all six framework components. Of these, six were on cost-benefit, two
were on cost-effectiveness, two on cost-consequence, and one on cost-utility.
For the remaining studies, 16 were on cost-related outcomes, and five on input
costs. As for the categories described under each of the six framework
components, their patterns of usage among the 33 HIS studies are tabulated below (for more detail, see Bassi & Lau, 2013).
- Perspective – Most studies (87.9% or 29/33) were based on an organizational perspective, while 12.1% (4/33) were on society, and 3.0% (1/33) each on individual and payer. Note that the total count exceeds 100% as two studies had two perspectives each and therefore were counted twice.
- Time Frame – Over half (54.5% or 18/33) of the studies had time periods of one to five years. Of the remainder, 24.2% (8/33) had six to 10 years, 12.1% (4/33) less than one year, and 3.0% (1/33) each for less than six months, greater than 10 years and multiple time points, respectively.
- Options – Close to half (45.5% or 15/33) of the studies had options of with or without the system, while 27.3% (9/33) had pre- and post-implementation options. The remaining were 9.1% (3/33) on different types of options with similar functions, 9.1% for different levels of adoption, and 3.0% (1/33) each for different time points and not defined, respectively.
- Input Costs – 277 measures were reported based mostly on input cost analysis and cost benefit analysis studies. The majority of these measures were one-time direct costs (60.6% or 168/277) with the remaining as ongoing direct costs (32.9% or 91/277). Ongoing indirect costs were seldom mentioned (0.7% or 2/277). Of the 168 one-time direct cost measures, just over one-third (35.1% or 59/168) were for application development and deployment, with the remaining on hardware and software (32.1% or 54/168), initial data collection/conversion (6.5% or 11/168), initial user training (6.0% or 10/168) and other costs. Of the 91 ongoing direct cost measures, close to half were for IT and support staff salaries (25.3% or 23/91) and software licences, maintenance and upgrades (20.0% or 18/91). Many studies also had direct and indirect costs combined into other, overall and total costs.
- Outcomes – 195 measures were reported based mostly on cost-benefit analysis or cost-related outcome analysis studies. Close to half of the measures (46.7% or 91/195) were on resource utilization, mostly for medications (47.3% or 43/91) and laboratory tests (34.1% or 31/91). Other outcome categories include labour savings (17.4% or 34/195), healthcare service provision savings (12.3% or 24/195), and total costs/savings (12.8% or 25/195). Examples of labour savings reported are efficiency and time-related savings. Healthcare service provision savings refer to changes in clinical outcomes and include rates of adverse drug events, patient safety events and disease prevention or management. Total cost savings include such measures as annual cost savings, net benefit and incremental cost effectiveness ratio.
- Comparison of Options – Accounting was the most common method (72.7% or 24/33) used to compare options through such measures as the incremental cost-effectiveness ratios, return on investment, payback, net present value, net benefit, operating margin, least cost, average cost and cost savings. The estimation methods used to estimate future outcomes included linear/logistic regression (15.2% or 5/33), scenarios analysis (9.1% or 3/33), and general/linear modelling (9.1%). Many studies adjusted for inflation (30.3% or 10/33), discounting (24.2% or 8/33), and amortization/depreciation (12.1% or 4/33). Some studies applied statistical methods to test for differences among groups such as t-test (15.2% or 5/33), analysis of variance (6.1% or 2/33) and chi-square (3.0% or 1/33). Several studies used econometric or financial modelling methods based on simulation (12.1% or 4/33), parametric cost analysis (6.1% or 2/33), stochastic frontier analysis (3.0% or 1/33), and panel regression (3.0% or 1/33). For data sources, close to half (48.5% or 16/33) of the studies used both historical and published costs for comparison, while just over one-tenth (12.1% or 4/33) used historical and estimated costs. The remaining studies (39.4% or 13/33) used historical and estimated costs to project future costs and benefits.
5.5 Implications
The eHealth Economic Evaluation Framework described in this chapter can serve as
a classification scheme for the approaches used to evaluate the economic return
on eHealth system investments. The framework defines the six key components
that should be addressed when designing, analyzing and reporting eHealth
economic evaluation studies. There are four practice implications to be
considered when applying this framework: (a) the type of economic analysis
involved, (b) the use of estimated costs, (c) the importance of incremental
return, and (d) the issue of opportunity cost (Gospodarevskaya & Westbrook, 2014). These are described below.
- Type of economic analysis – From the scoping review we found only 12 studies were considered full economic evaluations with half of them being cost-benefit analysis, while the other types such as cost-utility analysis were rarely seen. The review included 16 cost-related outcome analysis studies that focused mostly on cost savings or cost changes after implementation. However, without knowing the initial costs of implementing the system it is difficult to determine whether the savings were worth the investment. Similarly, there were five studies on input cost analysis, which alone does not reveal the respective return on each option to make an investment decision.
- Estimated costs – Over half of the 33 studies in the review included some type of estimated costs when deriving the input costs or projecting cost-related outcomes. In general, economic evaluation studies that are based on expert opinions, cost avoidance and modelling should be viewed with caution. Expert opinions are subjective in nature and it is often difficult to validate their accuracy. Cost avoidance refers to potential reductions only and these are less convincing than tangible measureable outputs such as actual cost savings in dollars. Modelling studies are hypothetical in nature and may lead to unrealistic forecasts and expectations.
- Marginal return – Within the economics discipline, full economic evaluation is the comparative analysis of options that involves the identification, measurement and valuation of costs and outcomes to determine the incremental difference in costs in relation to difference in outcomes. This is demonstrated through the cost for each additional unit of outcome compared with an incremental cost-effectiveness ratio (ICER). In the review, only two studies applied ICER to determine the incremental return of the investment decision. The remaining studies compared the costs and outcomes for each option, which provides only an average cost-effectiveness ratio.
- Opportunity cost – Related to the notion of incremental return is the opportunity cost, which is the foregone benefit from the alternative use of resources beyond the eHealth system options. As such, the investment decision must demonstrate its economic efficiency by providing better value than the alternative use of resources and associated outcomes, including non-eHealth options.
5.6 Summary
This chapter described the eHealth Economic Evaluation Framework as a
classification scheme to help understand the different approaches used in
eHealth economic evaluation studies. The framework has six components: having a
perspective, options, time frame, input costs, outcomes, and method of
analyzing/comparing options. Best practice guidance does exist for each of the six
framework components and there are quality criteria for assessing such studies
that should be considered. By applying the framework components one can improve
the design, analysis, and reporting of eHealth economic evaluation.
References
Bassi, J., & Lau, F. (2013). Measuring value for money: A scoping review on economic
evaluation of health information systems. Journal of American Medical Informatics Association,20(4), 792–801.
Centre for Reviews and Dissemination (CRD). (2009, January). Systematic reviews —CRD’s guidance for undertaking reviews in health care. York, UK: University of York. Retrieved from http://www.york.ac.uk/crd/guidance
Drummond, M. F., & Jefferson, T. O. (1996). Guidelines for authors and peer reviewers of economic
submissions to the BMJ. British Medical Journal,313(7052), 275–283.
Evers, S., Goossens, M., de Vet, H., van Tulder, M., & Ament, A. (2005). Criteria list for assessment of methodological quality of
economic evaluations: Consensus on health economic criteria. International Journal of Technology Assessment in Health Care, 21(2), 240–250.
Gospodarevskaya, E., & Westbrook, J. I. (2014). Correspondence: Call for discussion about the
framework for categorizing economic evaluations of health information systems
and assessing their quality. Journal of American Medical Informatics Association,21(1), 190–191.
Husereau, D., Drummond, M., Petrou, S., Carswell, C., Moher, D., Greenberg, D., … Loder, E. (2013). Consolidated health economic evaluation reporting standards (CHEERS) – Explanation and elaboration: A report of the ISPOR health economic evaluation publication guidelines good reporting practices task
force. Value in Health,16, 231–250.
Machado, M., Iskedjian, M., & Einarson, T. R. (2006). Quality assessment of published health economic
analyses from South America. Annals of Pharmacotherapy,40(5), 943–949.
Roberts, M. S. (2006). Economic aspects of evaluation. In C. P. Friedman & J. C. Wyatt (Eds.), Evaluation methods in biomedical informatics (2nd ed., pp. 301–337). New York: Springer.
Annotate
EPUB